Originally posted in 2012, I’m sharing this again. I’ve learned so much more about the pump since this was written, and now believe that I was not a good candidate for this surgery. At this writing, I am still working on overcoming weakness that resulted from having the pump, and getting the pump removed.
Breaking Up Is Hard To Do
http://www.last.fm/music/Neil+Sedaka/_/Breaking+Up+Is+Hard+To+Do Bad Blood” soared to number one and went gold, and the album made the Top 20 and went gold, while also throwing off a new slow-tempo version of “Breaking Up Is Hard to Do” that peaked in the Top Ten in early 1976, leading to the odd occurrence that the 14-year-old tune earned a nomination for the 1976 Grammy Award for Song of the Year, which it lost to Bruce Johnston‘s “I Write the Songs.”
Is it time to find another neurologist? I’ve been seeing my current doctor for more than 18 years. He is a very nice man, and I like him. While eighteen years sounds like a very long time, it’s important to realize that for the first 7 or 8 years I only saw him occasionally, during a bad relapse, or when I first started on Betaseron.
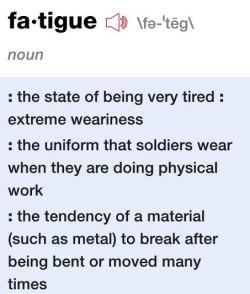
In those early years, I wasn’t so fond of him. The first bad relapse that I experienced as his patient was memorable, in that he WOULD NOT DO ANYTHING TO HELP ME. At the time, I had started a temporary tax-season job, and a few weeks into it, I developed profound foot-drop, fatigue, and my first occurrence of optic neuritis. I remember looking at my 10-key calculator, and right in the center of the key pad, there was a big, blue fuzzy spot, kind of like this:

I could look away and read the digits and the keypad fine; that is, peripherally I could see what I needed to, but I couldn’t look at anything normally and see it properly. I remember taking a stack of files, with tax returns I had completed, and walking to my boss’s office so he could review them. That started to feel difficult. One day, I left on my lunch hour, and stopped by a nearby park, thinking that maybe a little walk would be a good stress-reliever. Well, THAT was a huge mistake! I had only gotten about 25 yards when I felt my right foot dragging. I cried a lot that week; this is pretty scary stuff. By the end of the week, it was all I could do to get myself and my stacks of files to his office. I could feel the other staffers staring, but no one ever actually asked what was wrong. About mid-day that Thursday, I went home. The next day, I called in sick, and went to see my neurologist. I had been giving myself Betaseron injections for about 4 ½ months, and was distraught that this attack seemed so severe. The doc said it took at least 6 months to see the benefits of the drug: reduced attacks, or, relapses. Nobody can tell you that symptoms will go away, or when, and then the doc said, nope, no steroids for you! (Full disclosure: my understanding is that steroids do not affect the disease per se, but they do shorten an attack, i.e., lots of psychological reassurance, which I sorely needed.) Here is an image of what my doctor probably saw upon examination, when he shone that bright light into my right eye:  I went home and went to bed, not because I was tired, but really because I was so devastated at the recent turn of events. I didn’t return to work for another full 2 weeks. A neighbor taught at the school that my daughters attended, and she took them back and forth to school for me during this time.
I went home and went to bed, not because I was tired, but really because I was so devastated at the recent turn of events. I didn’t return to work for another full 2 weeks. A neighbor taught at the school that my daughters attended, and she took them back and forth to school for me during this time.
Miraculously (to me, anyway), after another 10 days or so, I returned to normal. The blue spot was gone! I could walk normally! It was as if nothing had ever happened! I went back to work, just in time for the final push to April 15, and I had the temerity to feel “saved.”
The following year, I returned to the work force full-time, and have worked ever since. In the intervening years, I saw my doctor more frequently. I had several more attacks. Apparently, the thinking changed, because he did order steroids for me on several occasions. I had a couple of MRI’s, and lots of discussions with him about symptomatic treatments, and tried other “disease-modifying” therapies. A few years ago, he revealed to me that he had a daughter-in-law with MS. How could that be anything but beneficial for me? The guy now has a vested interest in staying on top of the latest and greatest, right?
So, fast forward to now: I am unhappy with my doctor. It’s been a gradual realization, and even now, I’m trying to think very carefully about this. I live in a small city in the south, with only a handful of neurologists from which to choose. I commute to a nearby city, with more doctors, but regardless, none of these doctors specialize in MS: they’re all general neurologists. They see folks with Parkinson’s, ALS, migraines, and stroke sufferers. You have to go to a big city in a neighboring state to see an “expert” in MS.
Last year, my neuro recommended implantation of a Baclofen pump. I had that surgery (my first, ever), after a laborious process involving “pre-approval” by the insurance company, a spinal tap to “test” Baclofen on me, and consultation with a neurosurgeon. I called to schedule the filling of the pump with my neurologist, and still remember how irritated I was that he was out of town for a full week, just when the surgeon had removed the staples and I could actually begin to reap the benefits of all these efforts. I can still resurrect some anger that he and his staff did not organize things better for me. I mean, come on! He recommended the surgery. He suggested the neurosurgeon he wanted me to use (and I believe there was a clear motivation for his recommendation 1). Yet, I wound up in the position of trying to get his office to schedule me for filling the damn thing.
After a horrendous year during which I broke my ankle, and underwent surgery for THAT, I have made countless trips to this doctor to have adjustments made to my pump. Essentially, we’ve been titrating the dose of Baclofen, trying to achieve the right dose for me. It took me a few months to realize that this should have been expected: the whole process was delayed because of my injury. I spent a couple of months feeling like a “failure,” because it didn’t seem to be helping. I wish he had just said, look, you probably should plan on coming in every week or so, until we get the dosage right. Instead, as I tried to work, and rehabilitate my ankle, I would call his office and ask for a pump adjustment as I felt I could spare the time away from work. Finally, early this year, I’ve tried to make these appointments on my own. On more than one occasion, I scheduled a refill of the pump, only to be told upon arrival that, oh, no this is just an adjustment.
Sometimes they charged me a co-pay for these adjustments, and sometimes they didn’t. When I brought this up to the receptionist, she behaved as if I were nuts, saying, “That’s the only way we get paid!” Okay, fine, but why isn’t the procedure the same every time?
At one of these adjustments, I mentioned to the doctor that I needed to make a regular appointment to talk to him about other issues. He said that when I came in to have my pump refilled (about 2 months ago), there would be time then, as it was a 45 minute appointment. So I’m lying on the table, and his nurse is prepping me (there’s a whole kit to use for this process-sterile drape, the bits for getting the medication into the pump, swabs, etc.). Then the doc has this hand held device that reads the pump, including daily dosage, time to next refill, etc. It even prints out a narrow strip of paper with this information on it. But by the time all of this took place, time was up! I think I asked him about one treatment I’d heard about-Gilenya (read more here http://www.nationalmssociety.org/about-multiple-sclerosis/what-we-know-about-ms/treatments/medications/fingolimod/index.aspx), before he was off to his next patient.
Every time I need a refill of a certain prescription, they seem to call it in for only a 30-day supply. If I don’t remember to say, please write it for 90 days, I end up paying the higher price for the smaller supply. That means yet another call to his office, waiting on hold, explaining what I need to the receptionist, waiting for her to call me back, then contacting the pharmacy to pick it up.
Just last week, I scheduled a refill appointment, only to get a message two days later informing me that the receptionist scheduled “the wrong type of appointment,” and so rescheduled another date, 10 days later. As it happens, the entire week is booked solid with work events for me, and there’s no way I can make the “new” appointment time. I called them back today. They wanted to schedule me for the following week. “Well,” I said, “I’m pretty sure the alarm on my pump will go off before then.” (I didn’t shout it, or even put a virtual exclamation point at the end, but mentally, I was doing both! The pump has an alarm that goes off if it runs out of medication, because there are serious problems stopping the medication suddenly.)
Most people see an internist or a family practice doctor. I can’t remember the last time I was sick and went to see a “regular” doctor. I see my neurologist a lot. I do realize that a lot of this stuff is a product of, or is at least exacerbated by, our medical care system, specifically, for-profit insurance companies. (I refuse to call it our “health care system,” because it doesn’t seem to be about health, but about how to NOT pay for things. Another story altogether…)
Am I expecting too much for my doctor and his staff to help me manage my condition?
At the very least, I think they should be on top of this whole pump thing. Shouldn’t they? I mean, what if I blew it off as much as they seem to? If I were hospitalized because of the Baclofen running out, I wonder if he even visits patients in the hospital, with the recent advent of the “hospitalist.”
Is it really the patient’s responsibility to research the latest findings and ask about each one, with no prompting from the doctor? I am all for being informed, and I’m always reading and researching, but I am a layperson with no medical training whatsoever. I rely on my doctor to advise me.
Maybe it’s time for a new advisor.
1 There was no surgeon in my town who performed these surgeries at the time. My doctor prescribes Baclofen pumps for kids with cerebral palsy. Often, their caregivers refuse the surgery because they didn’t want to drive to a nearby city to have the surgery.

 trying to net the koi – not doing a good job
trying to net the koi – not doing a good job  our friend Rob (who really should think about keeping koi)
our friend Rob (who really should think about keeping koi)  Some of the larger koi were a two-man carry
Some of the larger koi were a two-man carry 
 I read several years ago that as we age, stretching becomes more difficult. Since my entire body seems to have become one big tight mess, I figure I better do everything I can.
I read several years ago that as we age, stretching becomes more difficult. Since my entire body seems to have become one big tight mess, I figure I better do everything I can. 


 I count myself lucky, because I experienced this before I had been diagnosed, but haven’t dealt with it since. Some people with MS have this on a regular basis, and despite the cute graphic, it is no fun at all.
I count myself lucky, because I experienced this before I had been diagnosed, but haven’t dealt with it since. Some people with MS have this on a regular basis, and despite the cute graphic, it is no fun at all. but many years ago, like this! : D
but many years ago, like this! : D